What is osteoporosis?
Osteoporosis is a condition that affects bone strength (the word osteoporosis literally means "porous bones"). Bone is made of collagen fibres (tough, elastic fibres) and minerals (gritty, hard material). It is a living tissue and contains cells that make, mould and resorb (take back up) bone. Initially, as you grow, bone formation exceeds bone resorption. But, as you get older, this reverses and, after about the age of 45, you start to lose a certain amount of bone material. Your bones become less dense and less strong. The amount of bone loss can vary. If you have a lot of bone loss, then you have osteoporosis. If you have osteoporosis, your bones can break more easily than normal, especially if you have an injury such as a fall. If you have a milder degree of bone loss, this is known as osteopenia.
How common is osteoporosis?
In the UK more than two million women are thought to have osteoporosis. Women lose bone material more rapidly than men, especially after the menopause when their levels of oestrogen fall. Oestrogen is a hormone and helps to protect against bone loss. At the age of 50, about 2 in 100 women have osteoporosis. This rises to 1 in 4 women at the age of 80. But, osteoporosis can also affect men. Over a third of women and one in five men in the UK have one or more bone fractures because of osteoporosis in their lifetime.
Who is at risk of osteoporosis?
All men and women have some risk of developing osteoporosis as they become older, particularly over the age of 60. As mentioned above, women are more at risk than men. The following situations may also lead to excessive bone loss and so increase your risk of developing osteoporosis. If you:
- Are a woman and you had your menopause before the age of 45.
- Have already had a bone fracture after a minor fall or bump.
- Have a strong family history of osteoporosis (that is, a mother, father, sister or brother affected).
- Have a body mass index (BMI) of 19 or less (that is, you are very underweight) - for example, if you have anorexia nervosa. In this situation, your levels of oestrogen are often low for long periods of time and, combined with a poor diet, this can affect bones.
- Are a woman and your periods stop for six months to a year or more before the time of your menopause. This can happen for various reasons. For example, over-exercising or over-dieting.
- Have taken, or are taking, a steroid medicine (such as prednisolone) for three months or more. A side-effect of steroids is to cause bone loss. For example, long-term courses of steroids are sometimes needed to control arthritis or asthma.
- Are a smoker.
- Have an alcohol intake of more than four units per day. (See separate leaflet calledRecommended Safe Limits of Alcohol for details of what a unit of alcohol is.)
- Lack calcium and/or vitamin D (due to a poor diet and/or little exposure to sunlight).
- Have never taken regular exercise, or have led a sedentary lifestyle (particularly during your teenage years).
- Have, or had, certain medical conditions. For example, an overactive thyroid, coeliac disease, Cushing's syndrome, Crohn's disease, chronic kidney failure, rheumatoid arthritis, chronic liver disease, type 1 diabetes or any condition that causes poor mobility.
Osteoporosis symptoms and problems
Osteoporosis usually develops slowly over several years, without any symptoms. However, after a certain amount of bone loss, the following may occur.
A bone fracture after a minor injury such as a fall
This is often the first sign or indication that you have osteoporosis. If you have osteoporosis, the force of a simple fall to the ground (from the height of a standard chair or less) is often enough to fracture a bone. A simple fall to the ground such as this does not usually cause a fracture in someone without osteoporosis. A bone fracture after a minor injury like this is known as a fragility fracture.
Fragility fractures are most commonly of the hip, wrist, and vertebrae (the bones that make up the spine). A fractured bone in an older person can have serious consequences in some people. For example, about half the people who have a hip fracture are unable to live independently afterwards because of permanent mobility problems.
Fragility fractures are most commonly of the hip, wrist, and vertebrae (the bones that make up the spine). A fractured bone in an older person can have serious consequences in some people. For example, about half the people who have a hip fracture are unable to live independently afterwards because of permanent mobility problems.
Loss of height, persistent back pain and a stooping (bent forward) posture
These symptoms can occur if you develop one or more fractured vertebrae. A vertebra affected by osteoporosis may fracture even without a fall or significant force on it. The vertebrae can become squashed with the weight of your body. If severe, a bent forward posture may affect your ability to go about your usual daily activities and may also affect your breathing, as your lungs have less room to expand within your chest.How is osteoporosis diagnosed?
Before any symptoms develop
The ideal situation is that osteoporosis should be prevented in the first place. If this is not possible, the next best thing is for diagnosis and treatment of osteoporosis as necessary before any symptoms or fracture occur.
At present, there is no national screening programme in the UK for osteoporosis. However, if you are a man over 50, or a woman over 50 who has gone through your menopause, your GP or other health professional may ask you questions to see how many risk factors for osteoporosis (listed above) apply to you. A risk calculator is available to determine your risk of developing osteoporosis depending on the number of risk factors that you have. If you are found to be at increased risk, or your risk is uncertain, you may be referred for a DEXA scan. DEXA stands for dual-energy X-ray absorptiometry. It is a scan that uses special X-ray machines to check your bone density. A DEXA scan can confirm osteoporosis.
At present, there is no national screening programme in the UK for osteoporosis. However, if you are a man over 50, or a woman over 50 who has gone through your menopause, your GP or other health professional may ask you questions to see how many risk factors for osteoporosis (listed above) apply to you. A risk calculator is available to determine your risk of developing osteoporosis depending on the number of risk factors that you have. If you are found to be at increased risk, or your risk is uncertain, you may be referred for a DEXA scan. DEXA stands for dual-energy X-ray absorptiometry. It is a scan that uses special X-ray machines to check your bone density. A DEXA scan can confirm osteoporosis.
After symptoms develop
Osteoporosis is often first diagnosed when you break a bone after a minor bump or fall. Even after the first fracture has occurred, treatment can help to reduce your risk of further fractures. If you are thought to have sustained a fragility fracture, you will usually be referred for a DEXA scan to look for signs of osteoporosis. However, sometimes women of 75 or older who have a fracture are assumed to have had a fragility fracture. In this group of women, treatment for osteoporosis may be started without having a DEXA scan first. This is because osteoporosis is so common in this age group.
Other tests
A newer test to look for osteoporosis is called digital X-ray radiogrammetry (DXR). It is easier to perform than a DEXA scan because it requires less technical equipment. It may sometimes be used as a screening test for osteoporosis - for example, in someone who has broken their wrist after a fall. However, it is not as sensitive as a DEXA scan at picking up all cases of osteoporosis. So, a DEXA scan remains the gold standard test.
What can I do to prevent osteoporosis?
The following may help to prevent, or slow down, bone loss. This advice is for everyone. But, it is particularly important if you are at increased risk of developing osteoporosis. If you already have osteoporosis, the following measures can also help to try to slow down any bone loss.
Exercise
Exercise can help to prevent osteoporosis. The pulling and tugging on the bones by your muscles during exercise helps to stimulate bone-making cells and strengthens your bones. Regular weight-bearing exercise throughout life is best, but it is never too late to start. This means exercise where your feet and legs bear your body's weight, such as brisk walking, aerobics, dancing, running, etc. For older people, a regular walk is a good start. However, the more vigorous the exercise, the better. For most benefit you should exercise regularly - aiming for at least 30 minutes of moderate exercise or physical activity at least five times per week. Excessive exercise such as marathon running may not be so good. (Note: because swimming is not weight-bearing exercise, this is not so helpful in preventing osteoporosis.)
Muscle strengthening exercises are also important. They help to give strength to the supporting muscles around bones. This helps to increase tone, improve balance, etc, which may help to prevent you from falling. Examples of muscle strengthening exercises include press-ups and weight lifting but you do not necessarily have to lift weights in a gym. There are some simple exercises that you can do at home.
See separate leaflet called Physical Activity For Health which gives more details about exercise.
Muscle strengthening exercises are also important. They help to give strength to the supporting muscles around bones. This helps to increase tone, improve balance, etc, which may help to prevent you from falling. Examples of muscle strengthening exercises include press-ups and weight lifting but you do not necessarily have to lift weights in a gym. There are some simple exercises that you can do at home.
See separate leaflet called Physical Activity For Health which gives more details about exercise.
Food and diet
Calcium and vitamin D are important for bone health. Your body needs adequate supplies of vitamin D in order to absorb (take up) the calcium that you eat or drink in your diet. The recommended daily intake for calcium in adults over the age of 50 is at least 1,000 mg per day. Everyone aged over 50 years should also aim for adequate amounts of vitamin D daily (800 IU). Protein is also important in your diet and one gram a day of protein per kilogram of your body weight is recommended. Briefly:
Calcium - you can get 1,000 mg of calcium most easily by:
Calcium - you can get 1,000 mg of calcium most easily by:
- drinking a pint of milk a day (this can include semi-skimmed or skimmed milk); plus
- eating 50 g (2 oz) hard cheese such as Cheddar or Edam, or one pot of yoghurt (125 g), or 50 g of sardines.
Bread, calcium-fortified soya milk, some vegetables (curly kale, okra, spinach, and watercress) and some fruits (dried apricots, dried figs, and mixed peel) are also good sources of calcium. Butter, cream, and soft cheeses do not contain much calcium.
Vitamin D - there are only a few foods that are a good source of vitamin D. Approximately 115 g (4 oz) of cooked salmon or cooked mackerel provide 400 IU of vitamin D. The same amount of vitamin D can also be obtained from 170 g (6 oz) of tuna fish or 80 g (3 oz) of sardines (both canned in oil). Vitamin D is also made by your body after exposure to the sun. The ultraviolet rays in sunshine trigger your skin to make vitamin D.
Some people over the age of 50 may need to take supplements if they are unable to get adequate amounts of calcium or vitamin D from their diet or sunlight. In fact, for most people aged over 65, an adequate amount of vitamin D can only be achieved by taking vitamin D supplements. For this reason, a dietary supplement of vitamin D is commonly recommended for people over the age of 65 and for others who may lack vitamin D. For example, people who have a poor diet, or people whose exposure to sunlight is limited, such as those who are largely housebound or women whose whole body is always covered by clothing. If you are unsure about whether you should havecalcium or vitamin D supplements, ask your practice nurse or GP.
Vitamin D - there are only a few foods that are a good source of vitamin D. Approximately 115 g (4 oz) of cooked salmon or cooked mackerel provide 400 IU of vitamin D. The same amount of vitamin D can also be obtained from 170 g (6 oz) of tuna fish or 80 g (3 oz) of sardines (both canned in oil). Vitamin D is also made by your body after exposure to the sun. The ultraviolet rays in sunshine trigger your skin to make vitamin D.
Some people over the age of 50 may need to take supplements if they are unable to get adequate amounts of calcium or vitamin D from their diet or sunlight. In fact, for most people aged over 65, an adequate amount of vitamin D can only be achieved by taking vitamin D supplements. For this reason, a dietary supplement of vitamin D is commonly recommended for people over the age of 65 and for others who may lack vitamin D. For example, people who have a poor diet, or people whose exposure to sunlight is limited, such as those who are largely housebound or women whose whole body is always covered by clothing. If you are unsure about whether you should havecalcium or vitamin D supplements, ask your practice nurse or GP.
Smoking and drinking
Chemicals from tobacco can get into your bloodstream and can affect your bones, making bone loss worse. If you smoke, you should try to make every effort to stop. Also, you should try to cut down on your alcohol intake if you drink more than three units of alcohol daily. Separate leaflets called Tips to Help you Stop Smoking andAlcohol and Sensible Drinking give further details.
Hormone replacement therapy
Hormone replacement therapy (HRT) contains oestrogen. A few years ago, HRT was widely used to prevent osteoporosis. However, the recent findings on the potential long-term health risks of HRT have meant that it is now not commonly used for this purpose (except in women who have had an early menopause). This is because of the small increased risk of breast cancer and cardiovascular disease (heart disease and stroke) if HRT is used in the long term.
Do I need treatment for osteoporosis?
If you have osteoporosis but have not had a fragility fracture, your doctor will be able to advise whether or not treatment is recommended in your case. They may use a special risk calculator to look at your risk of having a fragility fracture, to help with this decision. This incorporates things such as your age, your bone density measurements on a DEXA scan, and how many other risk factors for bone fractures or indicators for fragile bones you have(for example, any history in your family of hip fracture, how much alcohol you drink, your BMI, etc).
If you are found to have osteoporosis and you have already had a fragility fracture, treatment is usually recommended to help prevent a further fracture. The bisphosphonate drug alendronate is usually suggested first (see below). If alendronate is not suitable or not tolerated, other treatments may be suggested depending on things such as your age, your bone density measurements and how many other risk factors for bone fractures or indicators for fragile bones you have. Your doctor will be able to advise.
If treatment is started, repeat DEXA scanning on a regular basis may be suggested to look at how effective treatment is. Lifestyle measures and prevention of falls are important for all people with osteoporosis (see below).
If you are found to have osteoporosis and you have already had a fragility fracture, treatment is usually recommended to help prevent a further fracture. The bisphosphonate drug alendronate is usually suggested first (see below). If alendronate is not suitable or not tolerated, other treatments may be suggested depending on things such as your age, your bone density measurements and how many other risk factors for bone fractures or indicators for fragile bones you have. Your doctor will be able to advise.
If treatment is started, repeat DEXA scanning on a regular basis may be suggested to look at how effective treatment is. Lifestyle measures and prevention of falls are important for all people with osteoporosis (see below).
Medication for osteoporosis
Various drugs are available that can help to prevent and treat bone loss. Drugs used to treat osteoporosis include the follooporosis
Bisphosphonates
Bisphosponates are a group of drugs that includealendronate, risedronate and etidronate. They are the most commonly used drugs to treat osteoporosis. They work on the bone-making cells. They can help to restore some lost bone, and help to prevent further bone loss. Research studies have shown that the risk of bone fracture may be reduced by taking one of these drugs if you have osteoporosis. They may also help to reduce the chance of a second fracture if you have already had a fragility fracture.
Alendronate is the drug that is usually used first. Risedronate or etidronate may be considered in certain people who are not able to tolerate alendronate or in whom alendronate is not suitable.
Read the information sheet that comes with the drug, as you need to follow the instructions carefully on how to take a bisphosphonate. For example, you need to take bisphosphonate tablets whilst you are sitting up and with plenty of water, as they can cause irritation of your oesophagus (gullet). This can lead to indigestion-type symptoms such as heartburn or difficulty swallowing. Other side-effects may include diarrhoea or constipation. Also, you should not take bisphosphonates at the same time as food. Depending on which drug is used, you may need to take it daily, weekly, or sometimes less frequently.
A rare side-effect from bisphosphonates is a condition called osteonecrosis of the jaw. This condition can result in severe damage to the jaw bone. So, if you take a bisphosphonate and you experience pain, swelling or numbness of the jaw, a 'heavy jaw feeling' or loosening of a tooth, you should tell your doctor. Your should also brush and floss your teeth regularly and go for regular dental check-ups whilst taking a bisphosphonate. Tell your dentist that you are taking a bisphosphonate. Note: the risk of osteonecrosis of the jaw is low in people taking bisphosphonate tablets as a treatment for osteoporosis. It is greater in people with cancer who are being treated with bisphosphonates intravenously (into a vein).
Denosumab
This drug may be an alternative for women with osteoporosis who have been through the menopause if a bisphosphonate is not suitable or is not tolerated. It is given twice a year by injection and helps to slow down bone loss. Osteonecrosis of the jaw has also, rarely, been reported with this drug. However, it is thought that in the vast majority of people, the benefits of treatment outweigh the risks.
Raloxifene
Raloxifene is another option for some women with osteoporosis. It is usually only used if a woman has already had a fragility fracture. It works by mimicking the natural effects of oestrogen. This gradually reverses the excessive breakdown of bone that happens at the menopause and makes bones stronger. However, there may be a small increased risk of developing a deep vein thrombosis in some people who take raloxifene. You should discuss this with your doctor.
Parathyroid hormone peptide drugs
These drugs are sometimes suggested for people who have already had a fragility fracture. An example is called teriparatide. Studies have shown that they can reduce the risk of some osteoporotic fractures. But, they only tend to be used if other drugs cannot be tolerated or taken for some reason; or, if someone has been taking another treatment for one year and they have another fragility fracture and their bone density is getting worse.
Calcium and vitamin D tablets
Your body needs plenty of calcium and vitamin D to make bone. Unless your doctor is sure that you have an adequate intake of calcium and have enough vitamin D, they will often prescribe calcium and vitamin D supplements in addition to one of the above drugs.
Strontium ranelate
This is also used for treating osteoporosis. Research has recently shown that risks of this treatment may be worse than the benefits for some patients. For this reason the European Medicines agency has recommended that this medicine is only used if the patient is unable to take other types of prevention medicines. The patient should also have low risk of cardiovascular problems.
Other measures are also important
Lifestyle
Medication will not restore all lost bone. Also, medication may not be suggested for all people with osteoporosis. So, there are a number of lifestyle measures that are also important in treating osteoporosis. They include weight-bearing exercise, muscle strengthening exercises, not smoking, and keeping any alcohol drinking to within the levels as described earlier.
Preventing falls
You can also take measures to help prevent yourself from falling and breaking a bone.
- Check your home for hazards such as uneven rugs, trailing wires, slippery floors, etc.
- Regular weight-bearing exercise may help to prevent falls (as described above).
- Are your vision and hearing as good as possible? Do they need checking? Do you need glasses or a hearing aid?
- Beware of going out in icy weather.
- Do you take any drugs that can make you drowsy or that may lower your blood pressure too much and increase your risk of falls? Can they be changed? You can discuss this with your doctor.
- Hip protectors may also help in some people. These are special protectors that you wear over your hips that aim to cushion your hips if you do have a fall.
If you have had a fall, or have difficulty walking, you may be advised to have a formal falls risk assessment. This involves various things such as a physical examination, checking your vision, hearing, and ability to walk, reviewing your medication, and reviewing your home circumstances. Following this, where appropriate, some people are offered things such as a muscle strengthening and balance programme, or recommendations on how to reduce potential hazards in their home.
UGONJWA WA FIGO
 |
| Figo |
Magonjwa ya figo
Figo hufanya kazi muhimu mwilini ambazo ni:-
• Kudhibiti na kuhifadhi virutubishi na maji na kuondoa mabaki kupitia mkojo.
• Kuchuja damu ili kuondoa mabaki ambayo ni sumu mwilini. Baadhi ya mabaki hayo ni urea, uric acid, creatinine na ammonia.
• Kudhibiti viwango vya electrolyte mwilini, yaani Sodium (Na+ ) na Potassium (K+). Sodium husaidia kudhibiti wingi wa maji mwilini na pia huwezesha mawasiliano kati ya mfumo wa fahamu na misuli (enhances commucacation between brain/nerves and muscles).Potassium husaidia mapigo ya moyo between brain/nerves and muscles). Potassimu husaidia mapigo ya moyo (regulates heart beats) na kazi ya misuli (muscle function). Viwango vya kawaida kwa Sodium ni 135-145 mmol/L na Potassimu ni 3.5-5 mmol/L.
• Kudhibiti shinikizo la damu kupitia mfumo wa rennin-angiotension.
• Kutengeneza kichocheo cha Erythropoietin ambacho huchochea utengenezaji wa chembechembe nyekundu za damu.
• Kuchochea vitamin D ambayo hutumika katika kudhibiti kiwango cha Calcium na Phosphorous kwenye mifupa.
Iwapo mtu atapata ugonjwa wa figo ambao utaathiri figo zote mbili, kazi zote hizo hapo juu huathirika au kushindwa kufanyika kwa ufanisi na
madhara hutokea kutengemea kiwango cha athari. Figo zinaweza kushindwa kufanya kazi aidha kwa sababu za kipindi kifupi (acute renal failure) au kwa sababu za muda mrefu (chronic renal failure).
Sababu zinazoweza kufanya figo zishindwe kufanya kazi:
i) Katika muda mfupi:
o Upungufu mkubwa wa ujazo wa damu (kupoteza damu kwa kiasi kikubwa)
o Upungufu wa maji mwilini kutokana na kutapika, kuhara, na homa
o Matumizi ya baadhi ya dawa kama diuretics
o Mawe kwenye figo (kidney stones)
o Maambukizi kwenye figo mfano sepsis
o Uvimbe –uchungu (inflammation) kwenye mfumo wa uchujaji kwenye figo (acute glomerulonephritis)
o Uvimbe mkubwa wa tezi dume (prostatic hypertrophy)
o Saratani ya tezi dume (prostate cancer)
ii) Katika muda mrefu
o Kisukari kisichodhibitiwa
o Shinikizo kubwa la damu lisilodhibitiwa
o Uvimbe-uchungu wa kudumu kwenye mfumo wa uchujaji wa figo(chronic glomerulonephritis)
o Mawe kwenye figo
o Magonjwa ya tezi dume (Prostate disease)
Dalili za ugonjwa wa figo:-
Mwanzoni, ugonjwa wa figo hauoneshi dalili yeyote. Mara utendaji kazi wa figo unapopungua, dalili hujitokeza kuendana na udhaifu wa kudhibiti maji na electrolyte mwilini; kuondoa mabaki mwili; kutengeneza erythropoietin ambayo huchochea utengenezaji wa chembechembe nyekundu za damu, na pia udhaifu wa kuchochea Vitamini D ambayo ni muhimu katika kuweka viwango sahihi vya calcium-phosphorous kwenye mifupa, misuli na neva.
• Dalili za mwanzo ni kama:-
o Kudhoofika,
o Kuchoka mara kwa mara
o Kukosa nguvu,
o Kukosa pumzi/kupumua kwa shida
o Kuvimba mwili (hasa usoni), na
o Homa isiyokuwa kali
Hali hii isipogundulika mapema huweza kusababisha hatari ya kupoteza maisha.
• Udhaifu wa kutoa Sodium (Na+) mwilini husababisha wingi wa Sodium mwilini (hypernatremia) ambao huambatana na kujaa kwa maji mwilini (generalized oedema) kuongonzeka uzito ghafla, ongezeko la shinikizo la damu, kushindwa kupumua mwisho husababisha ugonjwa wa moyo (congestive heart failure).
• Udhaifu wa Potassium (K+) mwilini husababisha wingi wa potassium mwilini (hyperkalemia) ambao husababisha misuli kukosa nguvu au kuwa dhaifu na mapigo ya moyo kuenda ovyo ovyo (arrhythmias) na ikizidi huweza kusababisha kifo cha ghafla.
• Kushindwa kutolewa kwa urea mwilini husababisha uharibifu kwenye ubongo (encephalopathy).
• Udhaifu kwa ujumla husababishwa na upungufu mkubwa wa damu ambao husababishwa na kushuka kwa uwezo wa figo kutengenezaerythropoietin hivyo chembechembe nyekundu za damu kupungua.
• Kukosekana kwa uwiano unaotakiwa kati ya phosphorous na calcium huweza kufanya mifupa kuwa miepesi kuvunjika.
Ushauri wa lishe na ulaji kwa mtu mwenye ugonjwa wa figo
Ulaji wa mtu mwenye ugonjwa wa figo unapaswa kudhibitiwa kwa kiasi kikubwa kwani figo haziwezi tena kutoa mabaki ya protin, maji, chumvi na potassium kwa urahisi inapozidi mwilini. Vyakula vyenye chumvi na potassium nyingi viepukwe ikiwa ni pamoja na kuzingatia mambo yafuatayo:
Mambo ya kuzingatia katika ulaji:-
• Punguza kiasi cha nishati-lishe. Kiasi cha nishati-lishe na protini kinapozidi mwilini huzipatia figo ambazo zimeathirika kazi kubwa.
• Punguza kiasi cha vinywaji/vimiminika- ili kupunguza kujaa kwa maji mwilini ambako husababishwa na kushindwa kwa figo kutoa maji mwilini. Maji yakizidi mwilini husababisha kushindwa kupumua, shinikizo kuwa la damu, kuvimba mwili na huweza kusababisha
ugonjwa wa moyo (heart failure). Dhibiti ongezeko la uzito wa mwili kwani huweza kuonesha kuwa maji yamezidi mwilini.
• Punguza kiasi cha sodium: Kiasi cha maji mwilini hudhibitiwa nasodium. Pale sodium inapozidi mwilini husababisha maji kubaki mwilini. Hali hii huweza kusababisha ongezeko la uzito ghafla, kuvimba kwa viungio vya mwili, shinikizo kubwa la damu, kushindwa kupumua na huweza kusababisha ugonjwa wa moyo. Vyakula vyenye sodium kwa wingi ni vyakula vilivyosindikiwa kwa chumvi (nyama, samaki, soseji, bacon). Jenga tabia ya kutoongeza chumvi kwenye chakula wakati wa kula.
• Punguza kiasi cha potassium: Madini ya potassium yanapozidi mwilini husababisha misuli kuwa dhaifu na mapigo ya moyo kubadilika na yakizidi sana hueza kusababisha kifo cha ghafla. Ni muhimu kudhibiti kiasi cha potassium kwa ukaribu. Vyakula vyenye potassium kwa kiasi kikubwa ni pamoja na maparachichi, ndizi mbivu, maboga, machungwa, pichesi, peasi, matunda yaliyokaushwa na maharagwe. Vyakula vyenye potassium kwa kiasi kidogo ni pamoja na zabibu, machenza, mahindi mabichi, cauliflower, na matango.
Unaweza kupunguza kiasi cha potassium kwenye chakula kwa kuchemsha na kumwaga maji za ziada.
Kiasi cha potassium kinachoshauriwa kwa siku kwa mtu wa kawaida ni gramu 4.7 (milligram 4,700). Kwa mgonjwa wa figo inashauriwa gramu 1.5-2.7 (milligram 1500-2700) kwa siku na kila mlo asizidishe gramu 0.25 (miligramu 250).
• Punguza kiasi cha phosphorus
Uwiano wa calcium na phosphorus mwilini ni muhimu kuwezesha afya njema ya mifupa, misuli na neva. Phosphorus inapozidi mwilini mifupa huwa myepesi kuvunjika (brittle) na rahisi kuvunjika. Hii inatokana na mwili kutoa calcium kwenye mifupa vyakula ambavyo vina phosphorus kwa wingi ni pamoja na maziwa na mazao yake, nyama, shellfish, vyakula amvavyo havijakobolewa, maharage, karanga, korosho na chokoleti.
Vitamini na madini ya nyongeza
Wagonjwa wa figo huhitaji vitamin na madini ya nyongeza kutokana na kutokula aina mbalimbali za vyakula na hivyo kuweza kusababisha
upunfugu wa baadhi ya virutubishi. Damu inapochujwa (dialysis) pia huondoa vitamin kwenye damu. Virutubishi vya nyongeza vitolewe kwa mgonjwa wa figo kwa ushauri wa daktari.
SHINIKIZO LA DAMU AU PRESHA
Shinikizo la damu au presha ambalo kitaalamu huitwa Hypertension au High Blood Pressure ni neno la kitiba linalotumika kueleza hali ya ugonjwa wa shinikizo la juu la damu. Shinikizo la damu ni muhimu kwa ajili ya kusukuma damu katika sehemu zote za mwili, lakini shinikizo la damu la juu huweza kuleta matatizo na madhara makubwa kiafya. Shinikizo la damu kwa kawaida husababishwa na kuongezeka msukumo wa damu katika kuta za mishipa ya damu, hali ambayo huufanya moyo ufanye kazi zaidi kuliko kawaida ili kuzungusha damu mwilini. Shinikizo la damu huanishwa na namna damu inavyopiga kwenye kuta za mishipa ya damu. Kwa kawaida shinikizo la damu la mtu hupanda na kushuka kila siku, kwa baadhi ya watu hubakia juu na hapo ndipo huambiwa kuwa wana shinikizo la juu la damu. Ugonjwa huu kwa kawaida huitwa muuaji wa kimya kimya kwa maana kuwa, mtu anaweza akawa na ugonjwa huo kwa miaka kadhaa lakini bila kujua, huku ugonjwa huo ukimletea madhara makubwa. Njia ya pekee ya kujua iwapo una ugonjwa huu, ni kwenda kupimwa shinikizo lako la damu. Hii ni kwa sababu shinikizo la damu lisilodhibitiwa huathiri na kuharibu moyo, macho na figo na huongeza hatari ya kupata ugonjwa wa moyo na kiharusi.
Shinikizo la damu au presha huonyeshwa kwa muhtasari wa vipimo viwili vya sistoli na dayastoli, ambapo sistoli ni kipimo cha damu kinachopima nguvu ya msukumo wa damu katika mishipa ya damu wakati moyo ukidunda, na diyastoli ni kipimo cha damu kinachopima nguvu ya msukumo wa damu katika mishipa ya damu wakati moyo umepumzika au kati ya mapigo ya moyo. Shinikizo la damu hupimwa katika milimeta mercury. Kiwango cha kawaida cha msukumo wa damu pale mwili unapokuwa haupo katika harakati huanzia sistoli 100 hadi 140 mmHg na diyastoli 60 hadi 90 mmHg. Shinikizo la juu la damu ni pale vipimo hivyo vinapozidi mmHG 140/90.
&&&&&&&&
Shinikizo la damu limegawanyika katika makundi mawili, ambayo ni shinikizo la damu aina ya kwanza ambalo kitaalamu huitwa primary au essential hypertension. Aina hii ya shinikizo la damu huwapata asilimia 90 hadi 95 ya wagonjwa, huku sababu zikiwa hazijulikani suala linalomaanisha kuwa wagonjwa huwa hawana sababu za wazi zinazosababisha tatizo hilo. Kesi zinazobakia za shinikizo la damu ambazo ni asilimia 5-10 za wagonjwa husababishwa na shinikizo la damu aina ya pili, na kitaalamu huitwa secondary hypertension. Aina hii husababishwa na sababu mbalimbali zinazotokana na matatizo ya figo, mishipa ya damu, moyo na mfumo wa endocrine. Shinikizo la damu kwa kawaida huongezeka katika kipindi cha miaka kadhaa na huweza kumpata karibu kila mtu, lakini huwapata zaidi watu wazima wenye umri wa zaidi ya miaka 35. Sio vibaya kujua kuwa, zaidi ya Wamerakani milioni 50 wana ugonjwa wa shinikizo la damu, na Wamarekani wenye asili ya Afrika ndio wako kwenye hatari zaidi ya kupata ugonjwa huo. Sababu nyingi huathiri ugonjwa wa shinikizo la damu kama vile kiwango cha maji mwilini, kiwango cha chumvi mwilini, homoni, mishughuliko ya mtu, hali ya joto au hali ya baridi, hisia, hali ya figo, mfumo wa neva na mishipa ya damu. Iwapo shinikizo la damu litakuwa juu na kuachwa bila kudhibitiwa, moyo na mishipa ya damu kushindwa kufanya kazi ipasavyo. Kwa bahati nzuri, shinikizo la juu la damu ni rahisi sana kugunduliwa, kutibiwa na kudhibitiwa.
Pengine wengi tunajiuliza kuwa shinikizo la damu husababishwa na nini. Jibu ni kuwa, kuna sababu nyingi na zinazotofautiana kulinga na aina ya ugonjwa huo. Katika aina ya kwanza ya shinikizo la damuingawa chanzo huwa hakijulikani, lakini sababu za kijenetiki na za kimazingira kama chakula na mazoeni zina nafasi muhimu katika usababishaji wa ugonjwa huo. Hivyo masuala yafuatavyo yamehusishwa katika kusababisha aina hii ya shinikizo la damu. Masuala hayo ni uvutaji sigara, unene (visceral obesity) yaani unene wa sehemu za tumbo, unywaji pombe, upungufu wa madini ya potassium, upungufu wa vitamin D, kurithi, umri mkubwa, chumvi na madini ya sodium kwa ujumla, ongezeko la kemikali kwenye figo (renin) na kushindwa kufanya kazi kichocheo cha insulin.
Aina ya Pili ya shinikizo la damu husababishwa na tatizo lililopo mwilini. Matatizo hayo ni pamoja na kasoro ya kuzaliwa nayo katika mshipa mkubwa wa damu, saratani ya figo, saratani ya tezi iliyo juu ya figo, hali ya kushindwa kupumua vyema usingizini (sleep Apnea), ujauzito ambapo baadhi ya akina mama wajawazito hupata shinikizo la damu suala linalosababisha hatari ya kupata kifafa cha mimba (eclampsia), na pia magonjwa ya figo kama vile mshipa wa damu wa figo kuwa mwembamba yaani renal artery stenosis, matumizi ya baadhi ya dawa, madawa ya kulevya au kemikali, na kadhalika.
Tunapaswa kujua kuwa, mara nyingi shinikizo la damu huwa halina dalili zozote, na kama zikiwepo mgonjwa huhisi hali zifuatavyo: uchovu, maumivu ya kichwa, mapigo ya moyo kwenda mbio, kichefuchefu, kutapika, damu kutoka puani, kutoona vizuri (blurred vision), kupauka kwa ngozi au kuongezeka wekundu wa ngozi, kuhisi hali ya woga, kusikia kelele masikioni na mara chache kuchanganyikiwa.
Pale mtu anapokuwa na dalili za shinikizo la damu hupaswa kufanyiwa uchunguzi na vipimo vifuatavyo ili kuhakikisha kwamba ana tatizo hilo. Vipimo vya shinikizo la damu vinapatikana katika ofisi za madakatari na vituo vya afya, na huweza kupimwa na wajuzi mbalimbali wa afya. Ni muhimu kupimwa shinikizo la damu mara kwa mara (angalau mara moja kila baada ya mwaka mmoja au miwili). Unashauriwa kutokunywa vinywaji vyenye kafeini au kuvuta sigara kabla ya kupimwa shinikizo la damu. Kama shinikizo lako la damu liko juu, ni muhimu kumuona daktari ili kuweza kufanyiwa uchunguzi zaidi wa matatizo ya kiafya. Kipimo kimoja cha shinikizo la damu hakimaanishi kupatikana au kuugua ugonjwa huo, na inabidi kupimwa zaidi ya mara mbili. Huhitajia kupimwa angalau mara tatu tofauti, kwa wiki moja ili kuthibitisha kwamba mtu ana ugonjwa huo kwa kutumia kifaa maalumu cha kupimia shinikizo la damu kinachoitwa Sphygmomanometer.
Vipimo vingine ni pamoja na kuchunguza damu ili kufahamu wingi wa cholesterol mwilini na pia kupimwa BUN na electrolytes. Kipimo kingine ni cha kuchunguza mkojo, ECG, Echocardiography na pia Ultrasound ya mafigo.
&&&&&&&&
Baada ya vipimo kunyesha kuwa mgonjwa ana shinikizo la damu matibabu hufuata. Lengo la matibabu ni kuzuia madhara ambayo yanaweza kuletwa na shinikizo la damu. Kuna dawa mambalimbali zinazotumika kutibu shinikizo la damu kama dawa jamii ya Alpha blockers, dawa jamii ya Angiotensin converting enzyme inhibitor (ACEI), dawa jamii ya Angiotensin receptor blocker (ARB), dawa jamii ya Beta blocker, dawa jamii ya Calcium channel blocker, dawa jamii ya Diuretics yaani zile zinazopunguza maji mwilini au kuongeza mkojo, dawa jamii ya Renin inhibitors na pia Vasodilators.
Wapenzi wasikilizaji inafaa kujua kuwa, shinikizo la damu lisipotibiwa na kudhibitiwa husababisha madhara mbalimbali. Madhara hayo ni kama vile kiharusi, moyo kushindwa kufanya kazi, matatizo katika mshipa mkubwa wa damu ambapo ukuta wa ndani huchanika na damu kukusanyika katika ukuta wa mshipa huo, magonjwa ya mishipa ya damu, kushindwa kuona na pia huathiri ubongo.
Mbali na kutumia dawa tulizozitaja, tunaweza kuzuia na kudhibiti shinikizo la damu kwa njia tofauti
1) kula lishe bora na chakula kusichokuwa na mafuta mengi, na pia chenye madini ya potassium kitaalamu kinaitwa DASH diet ambacho ni maalumu kwa ajili ya kuzuia shinikizo la damu.
2) Kufanya mazoezi mara kwa mara, angalau nusu saa kwa siku.
3) Kuacha kuvuta sigara na kunywa pombe kwa wale wenye tabia hizo.
4) Kupunguza utumiaji wa chumvi nyingi katika chakula hasa ya kuongeza mezani (tunapaswa kutotumia zaidi ya gramu 1.5 ya chumvi kwa siku).
5) Kupunguza msongo wa mawazo.
6) Kuhakikisha kuwa tunakuwa na uzito unaotakiwa kiafya kulingana na kimo, na kama tuna uzito uliozidi tunapaswa kupunguza uzito huo ili uwe katika kiwango kinachotakiwa na 7) Kula samaki au kutumia mafuta ya samaki ambayo husaidia kupunguza shinikizo la damu, kwa wenye shinikizo la damu.
UJUE UGONJWA WA KISUKARI,DALILI ZAKE,MADHARA NA TIBA MBADALA
Kisukari (jina la kitaalamu: diabetes mellitus) ni ugonjwa unaoonyesha viwango vikubwa vya glukosi katika damu. Sababu yake ni uhaba wa homoni ya insulini mwilini au upungufu wa uwezo wa mwili wa kukubali insulini.
Dalili za kisukari ni
- kukojoa kupitia kiasi cha kawaida
- kiu kikubwa
- kuona vibaya na matatizo ya macho hadi kuwa kipofu
- kuchoka haraka
- vidonda vinavyopona polepole mno hasa kwenye miguu hadi kupoteza viungo
UGONJWA WA KISUKARI
Ugonjwa wa kisukari ni mlolongo wa matatizo mwilini,ya mda mrefu na mfupi kutokana na upungufu au kutoweza kutumika vizuri kwa kichocheo kinachoitwa insulin. Insulin hutengenezwa na chembechembe zilizopo ndani ya kiungo cha kongosho. Miili yetu inahitaji insulin ili kuweza kutumia sukari tuliyonayo mwilini. Sukari inatokana na ambacho tunakula kila siku na hutumika kwa kutupa nguvu mwilini. Kwa kawaida sukari ikizidi, ya ziada inahifadhiwa katika ini kama mafuta. Mafuta haya hubadilishwa kuwa sukari na kutumika wakati tukiwa na njaa kwa mda mrefu. Endapo kuna matatizo ya kutengeneza au kutumika kwa insulin, sukari mwilini huongezeka haraka na inamaanisha ugonjwa wa kisukari upo na dalili kuanza kuonekana.
Viashiria vya ugonjwa wa kisukari (risk factors)
- Unene uliozidi na kiribatumbo
- Ulaji mbaya wa chakula
- Baadhi ya madawa
- Msongo wa mawazo
- Historia ya ugonjwa wa kisukari kwenye familia
- Tezi ya shingo (husababisha mwili kukua na kuongezeka haraka)
- Kutofanya mazoezi
- Umri zaidi ya miaka arobaini (kadri tunavyozeeka na kongosho letu linapungua uwezo wa kutoa insulin hivyo kusababisha kisukari)
- Magonjwa yanayoharibu kongosho
- Akina mama wanaojifungua watoto wenye kilo zaidi ya arobaini (Mara nyingi hawa akina mama huwa na ugonjwa wa kisukari ila hawagunduliki hadi mtoto anapozaliwa na kuonekana mkubwa)
- Akina mama wenye historia ya kisukari wakati wa ujauzito
- Utumiaji uliozidia pombe na uvutaji sigara
Dalili za ugonjwa wa kisukari
· Kiu ya mara kwa mara
· Kupungua uzito licha ya kula vizuri
· Njaa kali na ya mara kwa mara
· Jasho jingi
· Uchovu usioeleweka hata bila kufanya kazi
· Kizunguzungu
· Macho kupungua uwezo wa kuona
· Kidonda kisichopona haraka
Tiba ya ugonjwa wa kisukari
- Tiba bila dawa- ukigundulika unatakiwa kula chakula utakachoshauriwa na kufanya mazoezi ili ili kushusha sukari yako iwe ya kawaida.
- Tiba kwa vidonge-wengine hawawezi kutumia chakula tu kwa kushusha sukari hivyo wanapewa dawa za vidonge ili kushusha sukari yao pamoja na chakula.
- Tiba kwa kutumia sindano ya insulin-wanopata kisukari kabla ya miaka 35 lazima watumie insulin ili kuishi. Pia wagonjwa wa umri zaidi ya miaka 35 inawezekane sukari yao isishuke kwa vidonge hivyo namna ya tiba yao inabaki kuwa sindano tu.
Madhara ya ugonjwa wa kisukari
Endapo ugonjwa wa kisukari utapuuzwa au kutotibiwa inavyostahili madhara mengi yanaweza kujitokeza na yanatokana na kiwango cha sukari kuwa juu mwilini.
- Magonjwa ya moyo
- Kiharusi
- Kupungua nguvu za kiume
- Figo kushindwa kufanya kazi
- Upofu
Ni matumaini yangu wewe msomaji umenufaika na hili somo na pia utanufaisha familia na jamii iliokuzunguka.
Kama hujapata huu ugonjwa ni muhimu kuepuka unene uliozidi kwa kula lishe nzuri na ya kiasi, epuka pombe, msongo wa mawazo, pombe na uvutaji wa sigara na la muhimu zaidi ni mazoezi ya viungo .
Tunashauriwa kupima kama tuna ugonjwa wa kisukari kila mwaka, hivyo basi nenda mapema ili kuepuka madhara. Pia unaweza kupiga simu namba 0653 883542 kujiunga na Clubthe Hope kwa afya,furaha na kutimiza ndoto zako
Diseases can cause a number of symptoms to any part of the body. Communicable diseases are ones that are spread by an infection when you come in contact with someone who has it. Noninfectious diseases do not spread and they are generally caused from genetics, environmental factors or deficiencies in nutrition.
Celiac Disease
Gluten is a protein found in rye, wheat, barley, and any product that is made with these grains such as bread, bagels, muffins, cakes, crusts and cookies. Celiac disease is a condition where the intestines suffer a bad reaction to gluten-containing products when they are consumed. The end result is stomach upset, diarrhea, bloating and pain in the joints.
Irritable Bowel Syndrome
Irritable bowel syndrome (IBS) is a condition where the muscles in the digestive tract do not function properly. Food ends up getting pushed along too quickly or too slowly. Symptoms that can take place with this noninfectious disease include intermittent bouts of diarrhea and constipation, bloating, gas, loss of appetite and emotional distress.
Cancer
Cancer comes in many forms and it can attack any part of the body. It is caused when healthy cells become mutated and they clump together to form tumors. There are many treatments for cancer, but there is no known cure. It is also noninfectious. According to the American Cancer Society, colorectal, breast, prostate and skin cancer were the most prevalent types of cancer in the United States in 2006.
Diabetes
When carbohydrates are eaten, they get converted to glucose which is blood sugar. To stabilize blood sugar levels, the pancreas releases insulin. In people that have diabetes, a noninfectious disease, the pancreas does not release insulin properly or at all in the most severe cases. This can cause kidney failure, blindness, nerve damage and heart problems.
Fibromyalgia
Fibromyalgia is a condition where an individual suffers chronic fatigue and his body can become very tender. Pain can be felt in the joints, muscles and various pressure points located behind the head, between the shoulder blades, on the inner knees, on the outer elbows and at the upper hips.
Narcolepsy
Narcolepsy is a chronic sleeping disorder that causes a major disruption in a person's life. According to the Stanford School of Medicine, this disease affects more than 1 in 2,000 Americans. It is characterized by a constant feeling of fatigue and sleepiness that can also include dream-like hallucinations and moments where the individual is paralyzed.
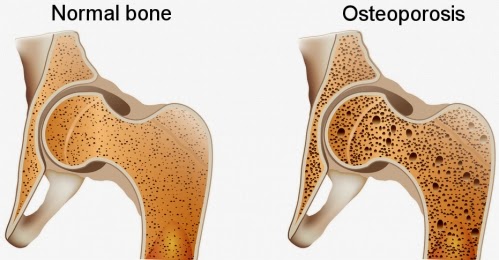
Osteoporosis
The bones require minerals and nutrients to stay healthy. They also need to be worked just like muscles to maintain their strength. If these variables are missing, a person can develop a condition called "osteoporosis." This is a noninfectious disease that most commonly takes place in older women and it is characterized by a low bone mineral density. Bones can become weak and brittle with this disease, and be more prone to getting fractured.


No comments:
Post a Comment